| Drug Name | GCC-CART |
| Description |
GCC-CART is human autologous T cells transduced with a lentiviral vector encoding a chimeric antigen receptor (CAR) targeting guanylate cyclase 2C (GUCY2C2). GUCY2C2 is a transmembrane protein that is expressed in the metastatic lesions of 70%-80% of subjects with colorectal cancers. GCC-CART is in early clinical development for the treatment of patients with relapsed or refractory metastatic colorectal cancer (mCRC). GCC-CART showed anti-tumor activities in vitro and in vivo experiments. Preliminary data from phase I clinical trials in the US and China show that pairing GCC-CART with CD19-targeting CAR T cells has significant efficacy and an acceptable safety profile in mCRC patients with mCRC. |
| Target | Guanylate cyclase 2C |
| Drug Modality | CAR-T cells |
| Indication | Metastatic colorectal cancer |
| Product Category | Cancer Immunotherapy |
| Mechanism of Action | Modified T cells activated by targeting GUCY2C2 to kill tumor cells |
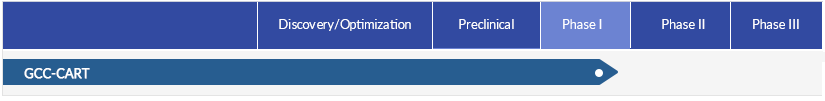
| Status | Phase I |
| Patent | Granted |
Protheragen Inc. is actively seeking partnership for GCC-CART. Potential collaboration can be strategic alliance, licensing, or marketing agreement.
We look forward to hearing from you.
| Introduction | Guanylate cyclase 2C, also known as guanylate cyclase C (GC-C) or heat-stable enterotoxin receptor (hSTAR), is a transmembrane protein encoded by the human GUCY2C gene. It belongs to the particulate guanylate cyclase class of receptors. GUCY2C consists of an amino-terminal extracellular domain, a single transmembrane helix, and a cytoplasmic region encompassing a kinase homology domain, a linker region, a catalytic domain, and a carboxy-terminal domain. GUCY2C is densely expressed throughout the intestine. In addition, GUCY2C is overexpressed on colorectal cancer cells and other gastrointestinal tumors, suggesting that this receptor is a promising tumor antigen for targeted therapy. |
| Approved Name | Guanylate cyclase 2C |
| Official Symbol | GUCY2C |
| Gene Type | Gene with protein product |
| Synonyms | STAR; HSER; GC-C; GCC |
| Ensembl | ENSG00000070019 |
| Gene ID | 2984 |
| mRNA Refseq | NM_004963.4 |
| Protein Refseq | NP_004954.2 |
| OMIM | 601330 |
| UniProt ID | P25092 |
| Chromosome Location | 12p12.3 |
| Gene Function | GUCY2C gene encodes a transmembrane protein that acts as a receptor for the endogenous peptides guanyin and uroguanylin, and the heat-stable Escherichia coli enterotoxin. The encoded protein activates the cystic fibrosis transmembrane conductance regulator. Mutations in this gene are associated with familial diarrhea (autosomal dominant) and meconium ileus (autosomal recessive). |
| Pathway | Guanylate cyclase signaling pathway |
| Major Conditions | Irritable bowel syndrome; Constipation; Colorectal cancer |
Chimeric antigen receptor-based T-cell (CAR-T) therapy is a type of cancer immunotherapy that has been successfully developed to the market for some B-cell malignancies, but there is currently no approved CAR-T cell therapy for the treatment of solid tumors, including colorectal cancer. GCC-CART is autologous T lymphocytes that are genetically engineered with lentiviral vectors encoding a CAR targeting guanylyl cyclase C (GUCY2C). GCC-CART cells are capable of recognizing the colorectal cancer-associated antigen GUCY2C independent of the expression of major histocompatibility complex (MHC) molecules, and hence of triggering an immune response directed toward the tumor.
Colorectal cancer (CRC) is a heterogenous malignancy involving various molecular pathways and genetic/epigenetic alterations that trigger the sequential transformation of normal mucosa to adenoma and then to carcinoma. Colorectal cancer is the third leading cause of cancer death and the second most important cancer-related cause of disability-adjusted life years worldwide.
Colorectal cancers are highly heterogeneous with respect to their aggressiveness, rate of progression, and malignant potential. Colorectal cancer typically develops over a period of several years and becomes a carcinoma with the capacity for further invasion and metastasis. The most frequent site of colorectal cancer metastasis is the liver. The five-year survival rate for patients with metastatic colorectal cancer is less than 15%.
The global incidence of colorectal cancer in 2019 was 2.17 million, and colorectal cancer caused 1.09 million deaths and 24.3 million DALYs worldwide, according to the Global Burden of Disease 2019 study. The global prevalence of colorectal cancer in 2020 was estimated at over 5.25 million, according to Globocan. According to an analysis of Globocan data from 185 countries, the estimated global lifetime risk of developing colorectal cancer was 3.16% in 2020. According to the IARC, colorectal cancer caused an estimated 904,019 deaths worldwide in 2022.
Surgery, radiotherapy and chemotherapy are the three pillars for the treatment of colorectal cancer. Although significant progress has been made in the treatment of colorectal cancer in recent years, a gold standard regimen is still lacking. First-line treatment of metastatic colorectal cancer consists of a chemotherapy regimen based on fluoropyrimidine, oxaliplatin and/or irinotecan, with or without therapies targeting vascular endothelial growth factor receptors (VEGFRs) or epidermal growth factor receptors (EGFRs). The objective response rates of Fegorafenib and Trifluridine-Tipiracil as third-line treatment ranged from 1% to 1.6%, with a median overall survival of 6-8 months.
Currently, conventional CAR-T cell therapy has shown weak cell expansion and achieved little or no therapeutic responses in patients with solid tumors. GCC-CART is an autologous CAR-T cell therapy developed based on a proprietary technology platform to treat relapsed or refractory metastatic colorectal cancer. GCC-CART is activated by specific binding to GUCY2C2, proliferates, and releases cytokines that promote the killing of GUCY2C2-expressing tumor cells. Compared with conventional CAR-T cells, GCC-CART pairing with CD19-targeting CAR-T cells shows improved expansion ability in vivo, enhanced migration ability, and resistance to immune suppression in the tumor microenvironment. The enhanced migratory capacity and resistance allow CAR-T cells to infiltrate tumor tissue sites and increase antitumor activity.
The safety, tolerability, clinical activity, pharmacokinetics and pharmacodynamics of GCC-CART is being evaluated in Phase 1 trial in the US for the treatment of relapsed or refractory metastatic colorectal cancer. Phase II clinical trial is expected to be initiated in 2025.